 Isobel Braithwaite The Healthy Planet delegation & support team for COP19 are having a twitter chat to discuss the recently released summary of the IPCC's 5th Assessment Report (Working Group 1) - you can download the summary of the IPCC AR5 summary here and more info on how we're planning to structure the chat here. The report is all about the climate science and includes projections of future temperature change, sea level rise and a discussion of other areas such as effects on oceans and air quality - and it makes for pretty depressing reading given the lack of significant action by governments, corporations or individuals, and George Osborne's cowardly and backward-looking stance that the UK shouldn't lead on climate change. The science and the inaction combine to create a lot of pretty worrying implications for health - but there is a good side too since there are many ways in which sustainability can benefit health - for example through active travel policy, clean energy and well-insulated homes. The section on human health is being released next year, and will be an update on the human health section from Assessment Report 4 in 2007 (available here). TIME magazine recently had a good piece on 'rebranding climate change as a public health issue' which highlighted some of the main impacts of climate change on health, and the scope for much greater impacts in the future. It showed how these aren't only in developing countries, although often the impacts are worst here - due to people's greater vulnerability and more limited opportunities for adaptation - with the example of Hurricane Sandy. At the same time, somewhere like New York is much better prepared and able to cope than, say, Tuvalu or Bangladesh. With rising sea levels and more evaporation, extreme weather events like Sandy are expected to become more frequent and more intense under climate change, as with flooding in general. Not only are there physical health consequences to events such as this, with potentially contaminated drinking water, exposure to cold and damp, reduced access to healthcare etc, but the mental health consequences of being displaced and losing property, and sometimes loved ones, can be immense and long-lasting. But climate change also affects health in more chronic ways, for example through long-term reductions in many regions' capacity to grow food because the growing temperatures are too high, and on top of this the effects of droughts, floods and the spread of crop diseases and pests to new places. Similarly, sea level rise, which is predicted to be at a faster rate and to reach 26-82cm higher than now by 2100, could force millions of people to migrate and increase the risks of coastal flooding and storm surges, causing loss of life directly as well as indirectly, eg. through crop losses and the spread of diseases like cholera and malaria. It can undermine people's livelihoods and contribute to migration and conflict, putting even more lives at risk, although typically this is in conjunction with many other drivers and near-impossible to attribute to climate change. 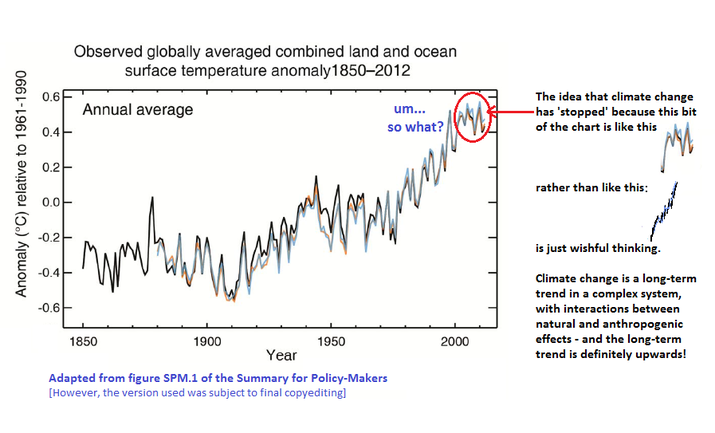 What about the 'hiatus' or 'pause' in warming that many skeptic groups are going on about and arguing is a sign that climate change won't continue? A recent article in Nature by Quirin Schiermeier quotes a co-chair of the report, Swiss climate scientist Thomas Stocker, at the launch of the report talking about the hiatus. According to Stocker, 'Comparing short-term observations with long-term model projections is inappropriate. We know that there is a lot of natural fluctuation in the climate system. A 15-year hiatus is not so unusual even though the jury is out as to what exactly may have caused the pause." It appears that deep oceans are taking up a lot of the excess energy that's being trapped, but Stocker's point that this is about long-term trends - and the last decade was the warmest on record - is important. Moreover, the real question is - do we need to be certain of something not to want to take that risk with future generations' health. We only have one planet and if this were and experiment, we'd never allow it. David Mitchell has a brilliant soapbox piece on this very topic (see below, worth a watch! And please ask us your questions and share your thoughts with us!! You can get in touch at [email protected]
0 Comments
 Alistair Wardrope, Healthy Planet Sheffield Originally posted here Would anyone dispute that healthcare systems ought to put their patients first? The mantra has a near-unassailable status in discussions of the best foundations for healthcare. The UK’s General Medical Council makes it first amongst the Duties of a Doctor; it provides the title of the Department of Health’s response to the findings of the Francis Report; and it lies (in its more-theorised form, ‘patient-centred care’) at the core of Don Berwick’s recent report into safety in the NHS. No politician, of any political stripe, would see fit to enter into a debate on health without it taking pride of place in their rhetoric. I’ve used it myself, campaigning for the priority of “patients before profits”. Nonetheless, I’ve long had qualms about it. It took a work of fantasy to figure out exactly why. During a recent and all-too-brief summer break, I decided to read China Miéville’s Perdido Street Station. I had harboured the vague intent of doing so for several years, but a fortuitous alignment of stars and an inability to access the books I was supposed to read in the university library meant I finally did. As a (somewhat lapsed) devotee of speculative fiction, I’d always expected to find more than simple escapism between its covers; however, I did not expect it to form the nucleus around which those nagging worries about patient-centred care would crystallise. The passage that set me thinking is little more than an aside, one of the short conversational detours the novel is littered with. It concerns a society of nomadic bird-people, the Garuda of Cymek. Garuda society is founded on the moral and political primacy of individual freedom. Their legal code admits but one crime – depriving another Garuda of choice; their ethical code, only one vice – disrespect. So far, so Tea Party. But the Garuda take these principles in an altogether different direction. Their interpretation of individualism rests on a particular understanding of what the individual is: the ‘concrete’ individual. As Ged, the autodidact librarian-priest, states: You are an individual inasmuch as you exist in a social matrix of others who respect your individuality and your right to make choices. That’s concrete individuality: an individuality that recognizes that it owes its existence to a kind of communal respect on the part of all the other individualities, and that it had better therefore respect them similarly. With the individual understood in these terms, disrespect becomes at heart a crime of ‘abstraction’: isolating one’s own individuality from the network of social interactions by which it and other persons are constituted and so losing the symmetry between them in which equal status is grounded. The Garuda share their ‘concrete’ understanding of the individual with a strong line of philosophers and political theorists. In his influential essay ‘Atomism’, the communitarian thinker Charles Taylor describes the individual as existing only when grounded in a society that affords the material, psychological and social resources for them to develop into freely-choosing agents, and provides the range of options necessary to make such choices meaningful. Respect for such individuals, therefore, is inseparable from respect for the social conditions underpinning their individuality. This is in stark contrast to the ‘atomism’ of the title, a charge he levels against the libertarian individual, whose values and preferences are interpreted and realised independently of others, and the protection of whose choices sets the boundaries of an acceptable social contract. These ideas are developed upon in recent work in feminist philosophy on ‘relational’ conceptions of autonomy. Traditionally, medical ethics has employed a rather thin understanding of autonomy – interpreted in the doctrine of informed consent, for example, as little more than decision-making capacity. Relational theorists argue that this ignores the role played by our emotions and attitudes towards ourselves and others – and their attitudes towards us – in developing and maintaining our capacities for autonomy. Consider an individual who, after a lifetime of oppression, comes to adopt those oppressive values as his own; the individual who does not have the necessary self-respect to consider herself worthy to make her own; or the individual who, like Aesop’s fox rejecting the inaccessible grapes as sour, comes to view certain ways of living as undesirable only because they are not realistic options available to them. In each case, the individual may be in full possession of the faculties that constitute mental capacity, but faces more subtle, relational, threats to their autonomy. The concrete individualism of the Garuda – and the work of communitarian and relational theorists – captures my concerns about patient-centred care. For in many interpretations of the term, the idea of the patient upon whom care is being centred is what the Garuda would consider an abstract individual. When patient-centredness merely means enhancing patient choice, increasing medical consumerism or a way to promote marketisation of health services, we present the patient as the isolated, rational ‘chooser’ that is the subject of Taylor’s ‘atomism’ critique. More generally, an interpretation of patient-centred care focussed solely on the clinical encounter – where it concerns only the interactions between health professionals and the individuals who come to them at the point of clinical need – risks leaving out other individuals and important aspects of care. When care is centred on the patient, who or what falls into the periphery? It seems to me that many who fall into the margins of this picture are those who are already most marginalised. Most obviously entering into this group are those who need health care but are unable to access it: ‘patient-centred’ care, focused on the abstract patient, has nothing to say about caring for those who – through legal, economic, social or psychological barriers to access – are unable even to become patients. But, even setting aside the tremendous injustice and inequity – where the most vulnerable communities, such as vulnerable migrants, refugees and asylum seekers, poor and oppressed groups, are done further harm –ignoring these groups is a public health disaster. Perhaps this could be remedied by defining ‘patients’ according to their need for health care rather than their ability to access it; but this picture still sees those patients as abstract individuals, and so has little room for public and global health concerns that make no sense in individualistic terms. Infection control, mitigation of climate change and its health impacts, social and political action on the social determinants of health: all are relational public goods. They are not focussed toward, or done in aid of, any individual patient, and only make sense at a population level. In the current political climate in the UK – where attempts are being made to limit access to healthcare for migrants, and such care is increasingly conceived of as a service provided to individuals for individual benefit – the rhetorical use of patient-centredness emphasises only the abstract patient, with the attendant dangers to public health sketched above. But the good news is that, when the individual is understood in concrete terms, these dangers are not just brought back into the fold – they become a central component of patient-centred care. The reason why is simple: the health of the individual simply cannot be considered in isolation from that of the population. As Sir Muir Gray writes, “personalised and population medicine are interwoven like warp and woof.” A healthcare intervention is never solely for a single, isolated patient; it is simultaneously a public health measure. So when the International Association of Patient Organisations puts patient involvement in social policy, universal access to health care, and attention to education, employment and family issues at the core of its definition of patient-centred care, it is not adding these in as an additional ingredient to aiding execution of the interests and desires of individual patients in the clinical setting. Rather, it acknowledges the former as a core component of the latter. And protecting and extending access to healthcare for migrants – economic, asylum seeker or undocumented – is not a good to be weighed against the health needs of a nation’s citizens, but an integral part of serving those needs. In meeting the challenges of shaping more environmentally sustainable health systems – able to meet the needs of people today without sacrificing those of future generations – we need not marginalise or ignore current patient’s interests; as elsewhere in healthcare improvement, “the greatest untapped resource in healthcare is the patient.” Such work on sustainable healthcare – the focus of this September’s CleanMed Europe conference in Oxford – is a re-interpretation of what patient-centred care could be, modelled on a more comprehensive understanding of what it means to be a patient. It turns out, then, that my concern is not primarily with putting patients first, or with patient-centred care – at least, not with what those ideals could and should mean. The problems arise only when the individual is considered in isolation from their social and political context and the environment around them. Given the fundamentally relational nature of health and disease, this isolation is intellectually and ethically untenable; patient-centred care makes sense only when we listen to the lesson I was taught by a fictional society – to view patients (ourselves included) as concrete, inherently social, individuals. |
Details
Archives
February 2019
Tags
All
|
 RSS Feed
RSS Feed
