By Connor Schwartz  Amartya Sen ponders justice Amartya Sen ponders justice Climate ethics and climate justice are subjects which hide in the background of COPs and treaties, rarely given any limelight of their own. In fact, the most common appeal to climate justice within negotiations are false ones, nations setting out their stall while grasping furiously for some foundations to stand it upon. Because, while the neoliberal hegemony of self-interested actors fails miserably to encompass the breadth of human social relations, it is demonstrably accurate on an international level. Powerful nations may appeal to political theory and forms of justice to back up their positions, but you can bet that their move went outcome first, evidence second, and not the other way around. For example, in the early 2000s while America was resisting becoming party to the Kyoto Protocol, the Bush administration argued furiously that the Annex 1 countries were being unfairly asked to mitigate a crisis which, all things considered, it looked like other countries had a lot more to lose from than themselves. Slowing anthropogenic climate change will cost us a packet and only benefit Tuvalu, how unjust! It did not matter, of course, that this claim is justified only by a philosophy so libertarian that no US president (Nixon included) has ever come close to it. No, much more important to scream “injustice!” and hope nobody really notices that the argument doesn’t stack up. Thus climate ethics has been sullied and debased by negotiators wanting a transcendent justification for their greed. It’s time to put it back at the heart of a global climate regime. Here is just one such attempt. It’s not perfect but I think it reveals a few key things we are looking for from a global climate treaty, and provides the beginnings of a move away from pragmatism and towards justice. Hold tight, here comes the theory. (If you’re not interested in the theory in isolation, jump straight to part two where climate change comes back onto the scene). When we discuss distributive justice of any kind, the first thing to be argued over is what’s called the “metric” – what exactly it is we should be distributing. Let’s narrow our gaze to egalitarianism – that equality is, for some reason, at least partially good – as it is now almost universally accepted across the liberal democracies. There are two traditional camps in the metric debate: resourcists and welfarists. As their names give away, resourcists believe justice includes a focus on equalising the amount of stuff people have, whereas welfarists prefer a focus on the wellbeing or happiness people get from that stuff. It’s the classic means/ends debate. This division has been standing for hundreds of years, splitting radical feminists from their traditional colleagues and communists from conservatives. This impasse however was, I believe, broken in 1979 when Amartya Sen – a heterodox development economist from Bangladesh – gave his Tanner Lecture entitled ‘Equality of What?’. In this lecture Sen dismantled both metrics, each with a simple thought experiment, asking whether what each model was forced to conclude sounded much like justice or not. Number one. Take two agents: one able-bodied and another with a severe disability needing round the clock care. Equalise resources. After covering their care expenditure, the disabled agent has far less resources than the able bodied agent to increase their wellbeing with. Similarly other divides – gender, social position, country of birth, etc. – reach the same conclusion: that a resource egalitarian looks to be saying that justice permits, or even requires, that wellbeing is determined by factors of luck. Ask yourself: does that sound much like justice? Number two. Brian is a plumber living in the city of London and Vikram works as a dabbawalla, distributing Tiffins to the workforce of Mumbai. Brian, from any objective standpoint, enjoys a far higher standard of living than Vikram yet it is certainly conceivable that Vikram is the happier of the two. Empirically, what’s called “hedonic adaptation” shows us that as our income increases so too can our expectations, resulting in no greater happiness. So say Vikram is the happier of the two because he expects less, and we have some spare resources to distribute. We must be persuaded to give the extra to Brian. Justice? To say a poor person has no claim to extra resources because their expectations are lower doesn’t sound much like justice to me. So what does Sen suggest? Justice, he claims, is found in neither resources nor welfare, but some function between the two, some measure of how we can translate resources into welfare. The correct metric for distributive justice is a person’s capabilities or, to be specific, the capability to achieve particular substantive human functionings. Say what? Put simply, what justice demands is equalised are the real and tangible freedoms that humans can possess. It doesn’t matter how much income a person has, if they have no access to healthcare then they are not being served by justice. It does not matter how happy a person is, if they cannot access education then that is a failure of justice.  Martha C. Nussbaum Martha C. Nussbaum Although the language of capabilities was introduced by Sen, it was American theorist Martha C. Nussbaum that developed it into a robust philosophical doctrine. Borrowing from the young Marx, Nussbaum claims that justice provides entitlement to a plurality of values that are both non-aggregable and non-fungible. In other words, we cannot serve justice by simply giving all a certain amount of a certain thing – say, money – and then leaving them to make choices as to how they trade it. Rather, we must concentrate on fulfilling a range of indicators that are distinct and cannot be traded off against each other. Simplistically, one could not for example be compensated for an inadequate life expectancy by being allocated more political rights. This stands explicitly against classical and neoliberal theories of development, relying on GNP to assess the growth of a nation and the wellbeing its peoples. What’s more we do not have to earn these entitlements. They are derived from our entitlement to “the respect and dignity of a life that is fully human”. We possess them, therefore, merely due to our species membership. (Nussbaum also holds that it is likely many other species are similarly entitled to various capabilities, but for now we can just consider our entitlements on account of our being human.) That’s all well and good, but what on earth does it have to do with climate negotiations? Lots, actually. Part two focuses on bringing climate change back into the picture, and putting justice back at the heart of a global climate regime.
1 Comment
 Alistair Wardrope, Healthy Planet Sheffield Originally posted here Would anyone dispute that healthcare systems ought to put their patients first? The mantra has a near-unassailable status in discussions of the best foundations for healthcare. The UK’s General Medical Council makes it first amongst the Duties of a Doctor; it provides the title of the Department of Health’s response to the findings of the Francis Report; and it lies (in its more-theorised form, ‘patient-centred care’) at the core of Don Berwick’s recent report into safety in the NHS. No politician, of any political stripe, would see fit to enter into a debate on health without it taking pride of place in their rhetoric. I’ve used it myself, campaigning for the priority of “patients before profits”. Nonetheless, I’ve long had qualms about it. It took a work of fantasy to figure out exactly why. During a recent and all-too-brief summer break, I decided to read China Miéville’s Perdido Street Station. I had harboured the vague intent of doing so for several years, but a fortuitous alignment of stars and an inability to access the books I was supposed to read in the university library meant I finally did. As a (somewhat lapsed) devotee of speculative fiction, I’d always expected to find more than simple escapism between its covers; however, I did not expect it to form the nucleus around which those nagging worries about patient-centred care would crystallise. The passage that set me thinking is little more than an aside, one of the short conversational detours the novel is littered with. It concerns a society of nomadic bird-people, the Garuda of Cymek. Garuda society is founded on the moral and political primacy of individual freedom. Their legal code admits but one crime – depriving another Garuda of choice; their ethical code, only one vice – disrespect. So far, so Tea Party. But the Garuda take these principles in an altogether different direction. Their interpretation of individualism rests on a particular understanding of what the individual is: the ‘concrete’ individual. As Ged, the autodidact librarian-priest, states: You are an individual inasmuch as you exist in a social matrix of others who respect your individuality and your right to make choices. That’s concrete individuality: an individuality that recognizes that it owes its existence to a kind of communal respect on the part of all the other individualities, and that it had better therefore respect them similarly. With the individual understood in these terms, disrespect becomes at heart a crime of ‘abstraction’: isolating one’s own individuality from the network of social interactions by which it and other persons are constituted and so losing the symmetry between them in which equal status is grounded. The Garuda share their ‘concrete’ understanding of the individual with a strong line of philosophers and political theorists. In his influential essay ‘Atomism’, the communitarian thinker Charles Taylor describes the individual as existing only when grounded in a society that affords the material, psychological and social resources for them to develop into freely-choosing agents, and provides the range of options necessary to make such choices meaningful. Respect for such individuals, therefore, is inseparable from respect for the social conditions underpinning their individuality. This is in stark contrast to the ‘atomism’ of the title, a charge he levels against the libertarian individual, whose values and preferences are interpreted and realised independently of others, and the protection of whose choices sets the boundaries of an acceptable social contract. These ideas are developed upon in recent work in feminist philosophy on ‘relational’ conceptions of autonomy. Traditionally, medical ethics has employed a rather thin understanding of autonomy – interpreted in the doctrine of informed consent, for example, as little more than decision-making capacity. Relational theorists argue that this ignores the role played by our emotions and attitudes towards ourselves and others – and their attitudes towards us – in developing and maintaining our capacities for autonomy. Consider an individual who, after a lifetime of oppression, comes to adopt those oppressive values as his own; the individual who does not have the necessary self-respect to consider herself worthy to make her own; or the individual who, like Aesop’s fox rejecting the inaccessible grapes as sour, comes to view certain ways of living as undesirable only because they are not realistic options available to them. In each case, the individual may be in full possession of the faculties that constitute mental capacity, but faces more subtle, relational, threats to their autonomy. The concrete individualism of the Garuda – and the work of communitarian and relational theorists – captures my concerns about patient-centred care. For in many interpretations of the term, the idea of the patient upon whom care is being centred is what the Garuda would consider an abstract individual. When patient-centredness merely means enhancing patient choice, increasing medical consumerism or a way to promote marketisation of health services, we present the patient as the isolated, rational ‘chooser’ that is the subject of Taylor’s ‘atomism’ critique. More generally, an interpretation of patient-centred care focussed solely on the clinical encounter – where it concerns only the interactions between health professionals and the individuals who come to them at the point of clinical need – risks leaving out other individuals and important aspects of care. When care is centred on the patient, who or what falls into the periphery? It seems to me that many who fall into the margins of this picture are those who are already most marginalised. Most obviously entering into this group are those who need health care but are unable to access it: ‘patient-centred’ care, focused on the abstract patient, has nothing to say about caring for those who – through legal, economic, social or psychological barriers to access – are unable even to become patients. But, even setting aside the tremendous injustice and inequity – where the most vulnerable communities, such as vulnerable migrants, refugees and asylum seekers, poor and oppressed groups, are done further harm –ignoring these groups is a public health disaster. Perhaps this could be remedied by defining ‘patients’ according to their need for health care rather than their ability to access it; but this picture still sees those patients as abstract individuals, and so has little room for public and global health concerns that make no sense in individualistic terms. Infection control, mitigation of climate change and its health impacts, social and political action on the social determinants of health: all are relational public goods. They are not focussed toward, or done in aid of, any individual patient, and only make sense at a population level. In the current political climate in the UK – where attempts are being made to limit access to healthcare for migrants, and such care is increasingly conceived of as a service provided to individuals for individual benefit – the rhetorical use of patient-centredness emphasises only the abstract patient, with the attendant dangers to public health sketched above. But the good news is that, when the individual is understood in concrete terms, these dangers are not just brought back into the fold – they become a central component of patient-centred care. The reason why is simple: the health of the individual simply cannot be considered in isolation from that of the population. As Sir Muir Gray writes, “personalised and population medicine are interwoven like warp and woof.” A healthcare intervention is never solely for a single, isolated patient; it is simultaneously a public health measure. So when the International Association of Patient Organisations puts patient involvement in social policy, universal access to health care, and attention to education, employment and family issues at the core of its definition of patient-centred care, it is not adding these in as an additional ingredient to aiding execution of the interests and desires of individual patients in the clinical setting. Rather, it acknowledges the former as a core component of the latter. And protecting and extending access to healthcare for migrants – economic, asylum seeker or undocumented – is not a good to be weighed against the health needs of a nation’s citizens, but an integral part of serving those needs. In meeting the challenges of shaping more environmentally sustainable health systems – able to meet the needs of people today without sacrificing those of future generations – we need not marginalise or ignore current patient’s interests; as elsewhere in healthcare improvement, “the greatest untapped resource in healthcare is the patient.” Such work on sustainable healthcare – the focus of this September’s CleanMed Europe conference in Oxford – is a re-interpretation of what patient-centred care could be, modelled on a more comprehensive understanding of what it means to be a patient. It turns out, then, that my concern is not primarily with putting patients first, or with patient-centred care – at least, not with what those ideals could and should mean. The problems arise only when the individual is considered in isolation from their social and political context and the environment around them. Given the fundamentally relational nature of health and disease, this isolation is intellectually and ethically untenable; patient-centred care makes sense only when we listen to the lesson I was taught by a fictional society – to view patients (ourselves included) as concrete, inherently social, individuals. By Shuo Zhang 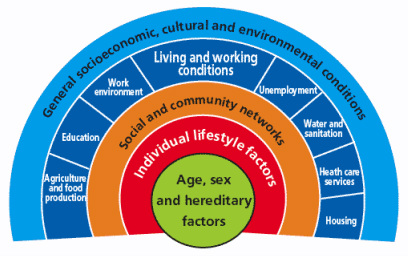 Dahlgren and Whitehead model (1991) of the determinants of health [6] First published in 'Art of the Possible - the Cambridge Journal of Politics' 2011-02-13 2010 saw a year of spending cuts, riots about public sector reforms and a shift in rhetoric away from “big government” to “big society”. Fundamentally, according to the Coalition Government’s vision, the state needs to move towards leaner, meaner public services and greater freedom and individual choice. This social, institutional and political change has implications for the National Health Service (NHS) in direct and indirect ways, both as a result of the 2010 Health White Paper1 and through the impact on other services that influence wider social determinants of health. Doctors have had a mixed reaction to the new ideas, getting caught up in enticing vocabularysuch as choice and power. However, most have concerns about the risks associated with implementation. The profession faces many challenges in the years to come, not only due to changes in the demography of disease, but also changes in pensions, employment rights and training, technological and scientific innovations, and new emphasis on sustainable practice and preventative medicine. So how has the new Coalition Government approached health and will it meet the challenges for the future? Healthcare is assumed to be a pillar of society and, even in this climate of austerity, the Coalition is keen to be seen to protect the NHS. The 2010 White Paper promises real-term increases in funding, although it also stipulates the need to move towards greater efficiency and cost savings of £20 billion in the next few years. Beyond the economics, the new Health White Paper advocates structural institutional change and a shift in power towards patients and frontline professionals. In addition, public health is to become more integrated with local councils. These proposals have underlined tensions and contradictions that touch upon wider political debates about how the country should navigate this period of hardship.2 One of the most significant proposals is the introduction of the GP-led commissioning service and greater choice for patients when registering with providers. This aims to move control away from managers and towards people who know and use the system the most. This has parallels with existing patient-led support services and health activism that has broadened the health service into a user-provider network, replacing previous patriarchal structures. As an idea, a new directive that empowers patients should be welcomed; it allows them to take their health into their own hands, and could produce a system that is pro-health instead of anti-ill health. In practice, however, the implementation of these proposals may have unintended effects, such as changing the dynamics of the patient-doctor relationship, diverting more time away from patient care due to increases in paperwork and leaving the back door open for potential privatisation. This patient empowerment may also be too far down the line, and only after bad lifestyle choices have already been made, to make much difference to prevention. Furthermore, choice is often just a buzz word for the middle classes, and by creating a system whichpriorities the most vocal needs, hidden inequalities in access and treatment may emerge. A change that perhaps makes more sense is the reconstitution of public health to local authorities. This moves the remit of action for local authorities further up the chain and gives them a greater role in co-ordinating approaches across diverse sectors such as transport and education.3 In effect, it replicates approaches to public health from Victorian England when it formed a central part of town planning. This move will give the medical profession greater powers to address broader social determinants of health, but may also leave it more exposed to criticisms of state ‘nannying’. The government has also failed to consider the continuity of public health in both a community and clinical setting. Public health in clinical practice is vital in providing evidence and improving practice. Moving responsibility for aspects of public health to local councils may create discontinuity and compromise broader goals. The ring-fencing of public health funding under the Coalition signals their intention to continue to address inequalities in access and care; however, this contradicts the cuts to departments in key peripheral areas such as social care and education. To carry on business as usual is not an option. However, the proposed changes were not part of a natural evolution based around principles of adaptation and mitigation, but more of a reactionary event to a system already perturbed. The Coalition’s vision lacks coherence, and there are other ways forward in which power could be better balanced between organizations and individuals. The perspective I have gained from being involved with the climate change and health movement is one of pushing forward change and alternatives to the big picture in a subtle way: changing the way we think about health systems and social structure, changing our behaviour, and seeing savings in efficiency as opportunities rather than cuts.4 It is also a direction which embodies the ethos of ‘prosperity without growth’5 and is careful of the wider political and socio-determinants of health6. The movement realised that it had to re-frame climate change as simply an evolution for the better. For example, infrastructural and efficiency changes will have direct financial savings, with a reduction in emissions as an added bonus. On a personal level, eating less red meat and dairy products, and cycling more will have a primary health benefit as well as positive environmental impacts. In a way, we were trying to change people’s behaviour and thoughts without loading it with values and ideology. Big and, more importantly, sustainable differences can be made if small changes in perspective occur across the board. Ultimately, the danger is that the Coalition Government’s changes are ideologically driven instead of evidence-based. For these changes to be unleashed on an organization that employs 10 per cent of Britain’s workforce without initial trialling is a huge risk. If these structural changes do come into effect it will impact upon fundamental relationships between science, policy and the public. These spheres of influence, which are illustrated by figure 1, extend across individual, group and societal levels. The Coalition should be more aware of these connections. Have they done enough to ensure healthcare will be fit for the future or should we too be protesting for a new way forward? References 1 Department of Health, Equity and excellence: Liberating the NHS - Health White Paper 2010, London: The Stationery Office, 2010. 2 British Medical Journal, “More brickbats than bouquets?”, British Medical Journal, 341 (2010): c3977. 3 Anthony Kessel and Andy Haines,“What the white paper might mean for public health”, British Medical Journal, 341 (2010): c6623. 4 Muir Gray and Frances Mortimer, “Transforming Clinical Practice”, Sustainability for health: An evidence base for action, 2 December 2009. http://www.sustainabilityforhealth.org/clinicaltransformation/opinion-pieces/transforming-clinical-practice, accessed 10 January 2011. 5 Tim Jackson 'Prosperity without Growth' (2009) Routledge ISBN-10: 1849713235 http://www.amazon.co.uk/Prosperity-without-Growth-Economics-Finite/dp/1849713235 6 G Dahlgren, M Whitehead 'Policies and strategies to promote equity in health' (1991) World Health Organization. http://www.euro.who.int/__data/assets/pdf_file/0010/74737/E89383.pdf |
Details
Archives
February 2019
Tags
All
|

 RSS Feed
RSS Feed
